Understanding the Biomechanics of Traumatic Brain Injury to Find Treatments for the Injured
Barclay Morrison, an associate professor of biomedical engineering, compares the brain's physical response to traumatic brain injury to, of all things, a gelatin dessert.
“If you take a bowl of Jell-O and spin it rapidly, it wiggles inside the confines of the bowl, and as it wiggles, it stretches without changing volume, just like the brain,” he says.
All it takes is 40 milliseconds to sustain a life-changing brain injury. That blow to the head—or mechanical stimulus, as scientists call it—sets in motion a cascade of biological responses inside the skull responsible for the injury's devastating consequences.
There are more than 1.7 million head injuries in the United States each year, according to the Centers for Disease Control, but no treatment as yet for the progressive damage from brain trauma that can lead to disorders ranging from memory loss to Parkinson’s, Alzheimer’s and epilepsy.
Morrison and his team are tackling the problem by exploring the biomechanics of the brain and its response on a biological level to traumatic brain injury.
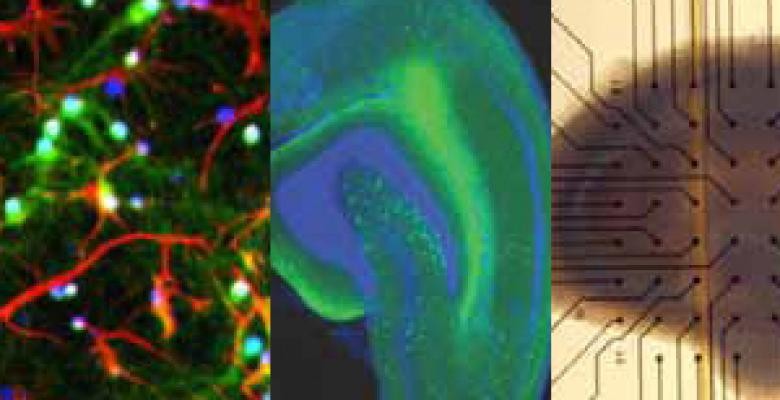
In his laboratory in Engineering Terrace, Morrison takes a silicone substrate, a flexible disk the thickness of a fingernail, cultures living brain tissue on it and stretches it over a metal tube to simulate the deformation of the brain during an injury. He tests how far tissue can stretch before neurons die and whether drug therapies can prevent cell death, with the ultimate goal of slowing or stopping the damage. He’s also studying the hippocampus, the region most vulnerable to brain injury and responsible for memory and learning, as well as the cortex, the largest part of the brain.
His lab has made progress recently on repetitive head injuries—when an initial injury causes little apparent damage but a subsequent blow soon after results in substantial harm. In research presented at the 2012 National Neurotrauma Symposium, Morrison showed that brain tissue after an initial injury treated with estrogen and memantine (a drug that is also used to treat Alzheimer’s symptoms) appeared to be more resistant when subjected to a second injury the next day. “We’re looking at treatments to break the synergy between two injuries,” Morrison says.
The work has potential applications in a number of fields besides athletics. One of Morrison’s research projects is a Department of Defense-sponsored collaboration with the University of Pennsylvania and Duke University. Its findings, which could be implemented within three to five years, could affect helmet design or regulations for how long a soldier should rest after being subjected to a blast from an improvised explosive device, for example. Another study sponsored by the National Highway Traffic Safety Administration focuses on providing insight into how the brain responds to different types of impact, research that could be applied to crash simulations for designing safer cars.
Morrison followed a family tradition into engineering, like his father and grandfathers before him. He grew up building model cars, planes and rockets, but was also fascinated with the brain and biology. Those interests led him to Johns Hopkins, where he studied biomedical engineering before getting his master’s and Ph.D. at the University of Pennsylvania. After a post-doc stint at the University of Southampton in Great Britain, he joined Columbia in 2003.
He got involved in traumatic brain injury while at Penn, whose medical school is home to the renowned Center for Brain Injury and Repair. “In graduate school when I was looking for a problem that would interest me, the combination of the biomechanics and biology of head injury is what drew me to it,” Morrison says.” Twenty years later, I'm still excited by that combination as we make progress reducing the socioeconomic costs of TBI."