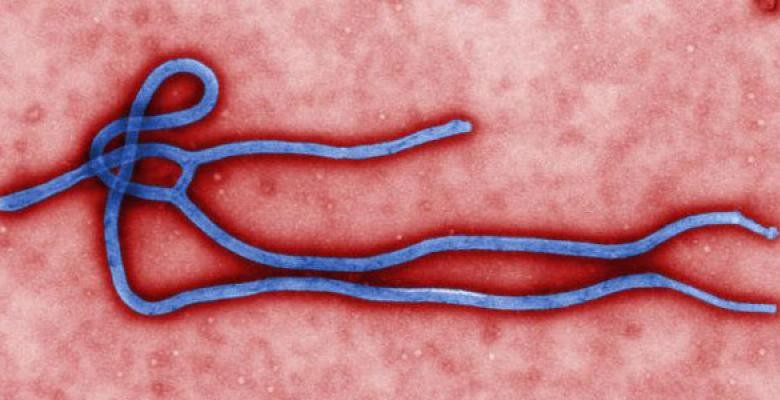
Columbia Experts Tackle Many Aspects of Ebola
On Nov. 11, Dr. Craig Spencer, New York’s first and thus far only diagnosed case of Ebola, was released from Bellevue Hospital Center where his recovery was made possible by expert care.
An alumnus of the Mailman School of Public Health and a physician at New York-Presbyterian/Columbia University Medical Center, Spencer had spent more than five weeks working with Doctors Without Borders to treat Ebola patients in Guinea. He is one of many Columbians, both faculty and students, who are working to prevent, contain, and treat the deadly illness.
Deans at Columbia Engineering and Mailman sponsored a rapid-fire design challenge that quickly yielded several products that could aid in the fight: a mobile platform for rapid response, patient care and data tracking; an Ebola-specific containment suit; and a blue-bleach solution to aid decontamination. Researchers led by Jeffrey Shaman, an associate professor of environmental health sciences at the Mailman School, have developed a computer model that tracks and forecasts the growth of cases in West Africa, the epicenter of the disease.
His team joins public health experts from Mailman and the Medical Center who are providing local and global authorities with a scientific basis for their policies and response. Epidemiologists, including Dr. W. Ian Lipkin and Dr. Abdul El-Sayed, are relaying their expertise to the news media and to a concerned public.
Shaman’s group provides status updates on the virus’ strength in West Africa. It forecasts cumulative infections and deaths six weeks ahead, which are generated each week and posted online. Much of his day is devoted to epidemiological measures such as the “basic reproduction number,” or R0, the projected number of cases generated by a single infected person in a fully susceptible population. If R0 falls below 1, the disease extinguishes itself. If it is greater than 1, it spreads—and the larger the number, the harder it is to control. Right now the R0 in the U.S. is close to zero.
Shaman spoke to Columbia News to answer some basic questions about the likely course of the disease.
Q: In September, your team developed a model to forecast the spread of the Ebola epidemic. What can it tell us about the spread of the virus?
We’ve been updating our site and forecasts each week as new data becomes available. In Sierra Leone, where the number of new cases grew exponentially in August and September, we have been forecasting continued exponential growth. In Liberia, there is some evidence of slowed growth, but this may reflect under-reporting of case levels. Future growth of the outbreak will depend on intervention and control efforts. The health systems in West Africa have been completely overwhelmed, so continued, aggressive support is needed from the developed world.
Q: What other factors affect the spread of a disease?
What’s made Ebola particularly hard to contain geographically is its incubation period—the time that you’re infected but in good health. It can be as long as three weeks before people become contagious. In each country you have a lot of mobility, so people can travel huge distances before any symptoms of illness appear. If the medical infrastructure isn’t built up and agile, which it isn’t, then there won’t always be the recognition needed to respond to the emergence of Ebola in a new location. In Liberia, the data indicate a slowing of the outbreak, but conditions on the ground call that data into question—it may still be growing but under-reported. As more resources like critical care hospitals, nurses and doctors arrive, hopefully this situation will improve.

Q: Concerns about the transmission of Ebola in the U.S. are considered overblown by most experts. How would you compare the basic reproductive number of Ebola in West Africa to that of the virus here?
If our infrastructure can respond appropriately—that is, isolate the infectious and those who have been in contact with the infectious, properly train and protect health care workers, and not let anyone slip through the cracks – then the basic reproduction number for Ebola in the U.S. should remain well below 1. However, this doesn’t mean there won’t be more imported cases. As long as the outbreak continues in West Africa, that risk will persist. In some sense, the West African Ebola outbreak is akin to a fire that has been allowed to spread and has grown much more difficult to extinguish.
Q: How long until response workers can extinguish it completely?
In the middle of the summer we were thinking this was going to be a six-to-nine month problem. In September, that estimate was revised to 12-18 months.
Q: You and your team also study the transmission of viruses in New York City. How does the spread of airborne upper respiratory viruses differ from the transmission of Ebola, which is spread through bodily fluids?
The short answer is we don't know. I would imagine that airborne viruses are more broadly dispersed, whereas something like Ebola is highly localized to infected persons and their immediate environment.
Q: How have you and your colleagues at Mailman and the Medical Center worked together to battle misconceptions about the virus?
It’s all about communication—taking the time to provide information to the public and quell rumors and fears. There have been many rumors about Ebola, both in West Africa and here. One common concern is that the virus will become airborne, but this is an incredibly remote possibility. This message needs to be repeated continuously.